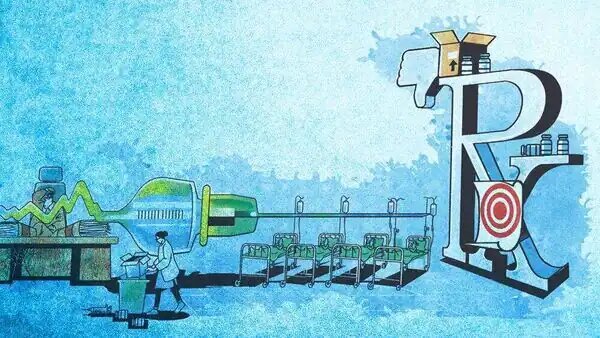
How did the state allow an ineffective vaccine to be administered to people for so long, despite being aware of its shortcomings?
BENGALURU : On 10 October 2022, Karnataka’s department of health and family welfare sent an odd circular to all of its district health officers. The circular, written in Kannada, spoke about the stock-out of a vaccine against the Kyasanur Forest Disease (KFD), a deadly disease that stalks mainly forest and agricultural workers. In light of this stock-out, no vaccine would be available for the upcoming November-May disease season of KFD, the circular said. And so, the health department asked the officers to control this tick-borne disease through other measures, such as educating people on how to avoid tick bites.
The circular was odd for several reasons. Also, the vaccine had been used in the state for some 33 years. So, why did the health department suddenly decide to stop using the vaccine?
What the circular didn’t reveal was that this decision, in fact, hadn’t been sudden. On the contrary, the vaccine had been riddled with both regulatory and quality problems for over two decades. Among these problems, India’s apex drug regulator, the Central Drugs Standard Control Organisation (CDSCO), had not given permission to the vaccine’s manufacturer, the Bengaluru-based Institute of Animal Health and Veterinary Biologicals (IAHVB), to make the KFD vaccine since at least 2002.
In other words, the sale of this vaccine in India had arguably been illegal for 21 years. These are the findings of a Mint investigation that began much before the October 2022 circular.
With the CDSCO missing from the picture, the vaccine’s quality had deteriorated measurably in the previous two decades. Specifically, the vaccine had been failing ‘potency’ tests repeatedly. The potency of a vaccine, which is measured in animals, is an indicator of how well the vaccine can prevent KFD in humans. In other words, potency is closely linked to the ‘effectiveness’ of the vaccine. So, if a vaccine fails a potency test, it means the vaccine may not be able to protect people well against KFD anymore.
Damningly, Mint uncovered atleast two instances in which the KFD vaccine’s manufacturer, IAHVB, and quality-testing laboratory, the Shivamogga-based Government Virus Diagnostic Laboratory (VDL), had released the vaccine to the public despite the vaccine failing potency tests. And the Karnataka health department had okayed these troubling decisions.
Nor had the IAHVB, VDL and the health department acted in isolation, Mint’s investigation found. Their decisions were enabled by one of the country’s top public health agencies, the National Institute of Virology (NIV). Mint learnt that NIV repeatedly suggested cosmetic-fixes to the problem of falling potency, instead of asking IAHVB to stop manufacturing altogether. In doing so, the NIV, which falls under India’s apex government medical-research organisation, the Indian Council of Medical Research, had helped the manufacturer release an ineffective vaccine to people.
Ultimately, people paid the price of this multi-level institutional failure. Historically, atleast five Indian states, namely Karnataka, Goa, Maharashtra, Tamil Nadu and Kerala, have purchased the KFD vaccine from IAHVB.
But these states were spending money on a shot that worked poorly, and whose quality and safety were questionable.
Studies conducted by the Chennai-based National Institute of Epidemiology show that the vaccine’s effectiveness had dropped dramatically by the mid-2000s. Using 2005-2010 KFD data, the National Institute of Epidemiology, a sister agency of NIV under the Indian Council of Medical Research, found that the effectiveness of one vaccine dose was zero during this period, compared to 79.3% in a 1994 study. Meanwhile, the effectiveness of two doses was a mere 62%, compared to 93.5% in 1994.
This meant that most recipients of a single dose were unprotected against the potentially deadly KFD. The disease, which sickens some 500 people annually in the Western Ghats regions of the affected states, is mild in most cases, characterised by fever and chills. But in 5-10% of patients, the virus can take a severe course, resulting in death. In severe disease, the virus impacts multiple organs, or causes haemorrhagic symptoms—like bleeding from the eyes, nose and intestines. Between 5 and 10% is not an insignificant case fatality rate; dengue, in comparison, kills around 2.6% of confirmed cases, as per one estimate.
The apparent loss of vaccine efficacy didn’t go unnoticed by healthcare workers in KFD-affected regions, many of whom lost confidence in the vaccine. “I don’t think it works,” Krishna (who goes by one name), a community health officer in the Kannangi village of Karnataka’s Shivamogga district, told Mint in a July 2022 interview.
The entire saga also raises questions about CDSCO’s performance as India’s national regulator, already in question after the deaths of 69 children in The Gambia, following the consumption of adulterated Indian cough syrup.
Mint learnt that even though the CDSCO was repeatedly made aware—since atleast 2020— about the KFD vaccine being used in Karnataka without its permission, the national regulator didn’t do anything to tackle the issue.
When Mint asked the Karnataka health department commissioner, Randeep Dev, in September, about the repeated releases of a failing vaccine, Dev said he couldn’t answer specific questions, because he wasn’t aware of historical details. However, he said the department had begun looking for alternative manufacturers, and would not release a vaccine again until its potency was proven.
In October 2022, the circular from his department finally stopped vaccine use, some two decades after the CDSCO stopped renewing permission to the manufacturer.
Even if Karnataka state finds a new manufacturer for the KFD vaccine, and solves the problems plaguing the shot, several questions will remain. How did the state allow an ineffective vaccine to be administered to people for so long, despite being aware of its shortcomings? How did the CDSCO and the Karnataka drugs control department look away in the face of blatant illegalities? Why was the NIV okay with common people getting a vaccine its own staff wouldn’t use? And will public faith in the vaccine, lost due to poor government decisions, ever come back?
Addtional Information:
Status of Manufacturing Permission of Human Vaccines till 2021
Link : https://cdsco.gov.in/opencms/opencms/system/modules/CDSCO.WEB/elements/download_file_division.jsp?num_id=NzY2Ng==
Source: Livemint